Why Your Soleus Muscle Could Be the Key to Pain-Free Knees and Stronger Legs
When people think of calf muscles, they often picture the bulging gastrocnemius—the part you can see. But underneath lies...
GLP-1 Medications: How They Work, Risks to Connective Tissues, and How to Protect Your Body
In recent years, GLP-1 receptor agonists—medications such as semaglutide (Ozempic®, Wegovy®) and tirzepatide (Mounjaro®,...
CoQ10 and Statins: Protecting Your Energy and Cellular Health
Statin medications are among the most commonly prescribed drugs worldwide, helping millions of people reduce high...
Perimenopause, Hormones, and Musculoskeletal Pain: What’s Happening—and What Helps
At Advanced Manual Therapies, we’ve noticed a pattern lately—many women in their 40s and early 50s walk through our doors...
Cold Water Immersion
Cold water plunging, or cold water immersion (CWI), has gained attention for its potential health benefits, including...
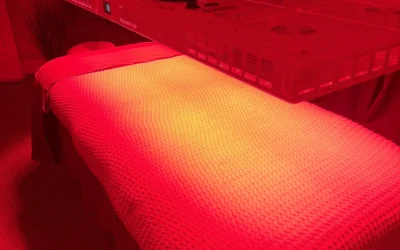
Red Light Therapy
Red Light Therapy (RLT), also known as low-level laser therapy (LLLT), is a non-invasive treatment that uses low wavelength...
Fiber: What Is It and Why Do We Need It?
Fiber is an essential component of a healthy diet, yet many people struggle to get enough of it from their food. Fiber is a...
The Importance of Sleep
Sleep is incredibly important to our physical and mental health. It helps to restore our energy levels, allowing us to be...
What are the benefits of Apple Cider Vinegar?
Helps with Weight Loss: Apple cider vinegar can help with weight loss due to its acetic acid content which may help reduce...